Combining the sciences to tackle health challenges: UTI diagnosis, social science and SLIC
Urinary tract infections (UTIs) are among the most common infections investigated in clinical settings, affecting more than 404.6 million individuals in 2019. These bacterial infections are usually treated with antibiotics, but a global rise in antimicrobial resistance (AMR) has meant that diagnosing and treating UTIs increasingly requires a high level of specificity, in order to ensure that the infection-causing bacteria are not resistant to the prescribed antibiotics.
The most accurate ‘gold standard’ form of testing is the culture method, which can diagnose the type of bacteria which a patient has and can inform clinicians of which antibiotic to use for treatment. This process takes three days and is costly – making it inaccessible to patients who live miles away from hospitals and those who cannot afford the diagnosis.
As such, hospitals in low-resource settings tend to rely on ‘rapid’ UTI diagnostic methods. However, these methods are low in both sensitivity and specificity, and their results are inadequate to inform antibiotic choice. Additionally, they are unable to identify the type of bacteria a patient is infected with, and they may fail to diagnose an infection (a false negative) – or falsely diagnose an infection when it is not present (a false positive). Faulty diagnoses result in faulty treatments, and thus patients can be prescribed medicine that is ineffective, given antibiotics that they do not need, or go untreated for their UTI.
Hellen Onyango is a medical laboratory scientist at Jomo Kenyatta University of Agriculture and Technology (JKUAT) in Kenya, specialising in medical microbiology. She is completing a PhD in the School of Medicine supervised by Drs Robert Hammond and Derek Sloan in Medicine, and Drs Katherine Keenan and Mike Kesby of the School of Geography and Sustainable Development.
Her GCRF-funded project tackles this problem of UTI diagnosis and treatment, using the scattered light integrating collector, or SLIC: a light scattering device developed by Dr Robert Hammond. Drawing on methods from both microbiology and the social sciences, Hellen’s fieldwork has consisted of analysing urine samples from patients presenting with symptoms suggestive of UTI in two government health facilities in Kenya and working with clinicians and lab technologists to explain and demonstrate the capabilities of SLIC. Hellen’s research is the first of its kind to bring this technology to Sub-Saharan Africa, presenting vast potential to influence healthcare provision across the region.
What is SLIC?
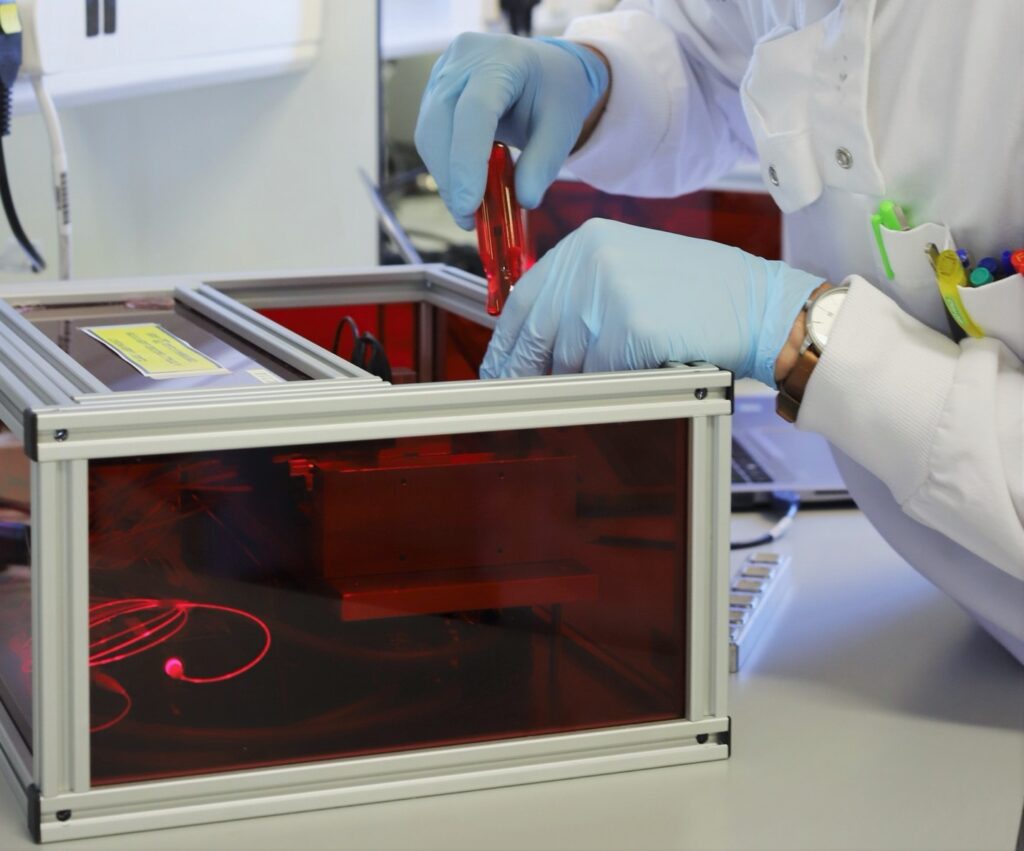
SLIC is a low-cost, laser-based technology that can monitor the growth of bacteria in vitro in real time. In a few minutes, it can detect the presence of bacteria in a urine sample. In under two hours (typically around 30 minutes), it can deduce the antimicrobial susceptibility of the bacteria to various antibiotics – a critical aspect to ensure effective treatment. SLIC provides a promising rapid bacterial detection strategy and offers the opportunity to significantly reduce the current timeframe for UTI diagnosis and the detection of resistance. Most importantly, this will promote good use of antibiotics (known as antibiotic stewardship) and improve patient outcomes.
SLIC works by first directing a laser at a sample. The laser’s light then scatters based on the number and morphology of bacteria cells in the sample, resulting into either growth (when bacteria is present in a sample) or no growth (no bacteria in sample). The amount of growth achieved (measured in decibels) determines whether or not the patient is infected. To gauge drug resistance, the antibiotics can be added to the urine samples, and again subjected to SLIC. This time, the growth of the bacteria with the added antibiotic can be tracked. If the bacteria continues to grow in the presence of an antibiotic, then health professionals can see that the antibiotic is ineffective. However, if the antibiotic appears to inhibit bacterial growth by over 50%, it is shown to be effective. This technology produces results with 95% accuracy, a number comparable to diagnosis and treatments from the ‘gold standard’ culture method.
SLIC and the Social Sciences
While SLIC is still a research-only tool at the moment, it has been very well received for its accuracy, time efficiency, and ease of use. Its capabilities are remarkable but implementing it for use will not be as simple as delivering machines to hospitals everywhere. This new tool will require uptake and behavioral changes from clinicians and laboratory technologists, raising a few questions: what are the existing diagnostic and antibiotic prescribing practices? How do healthcare workers perceive the utility of SLIC in improving diagnosis and prescribing?
While not a social scientist herself, Hellen found it was essential to ask these questions when considering how to realistically and successfully integrate SLIC into clinical settings. With guidance from her supervisors, Katy Keenan and Mike Kesby, she developed a feasibility study as part of her research, working with SLIC’s end users to understand how the machine could be best suited for different people – from the patient-facing, efficiency-oriented clinicians, to the operational concerns of the lab technologists. By engaging many perspectives, Hellen’s project supports more integrated management in healthcare settings, with all healthcare workers feeling like their perspectives are equally valued. She hopes that this will encourage greater collaboration and communication between roles throughout the process of diagnosis and treatment.
On a wider scale, Hellen’s project also supports the validation of SLIC as a medical diagnostic tool. Her project has generated data for SLIC that will form part of its database, which is used in the process of validating SLIC for clinical use. If it is validated, it may significantly contribute to the WHO’s Antimicrobial Stewardship Programme, which seeks to face the challenge of AMR by advocating for a ‘coherent set of integrated actions which promote the responsible and appropriate use of antimicrobials to help improve patient outcomes across the continuum of cares.’
With both regional and global reach, Hellen is carrying out research with enormous potential to transform healthcare practices through engaging technology, science, and people.